Working Group 1 of the Intergovernmental Panel on Climate Change (IPCC) published its contribution to the Sixth Assessment Report (AR6) in September. Climate Change 2021: The Physical Science Basis is the most comprehensive assessment of “new scientific evidence relevant for a world whose climate system is rapidly changing, overwhelmingly due to human influence” (IPCC, AR6 Ch1 p1). AR6 does not assess the science related to either the impacts on or vulnerability to human health from climate change, or adaptations required to mitigate those impacts and vulnerability (that is the remit of the IPCC’s Working Group 2, whose Report will be published early next year). Nevertheless, it does provide a preliminary climate science perspective on the relationship between global warming and health.
The word ‘health’ appears 233 times in the 3949 pages of the Report, covering five broad areas of intersection between health and global warming. Heat and air pollution are given most consideration, but drought, forest fires and mental health are also identified specifically, as is the need to engage the health community to help develop climate-health “storylines”. The data provided by AR6 for each of these intersections is summarised below and is presented as an entry point for discussion on global warming and health in the lead up to, and during, the two weeks of negotiation in Glasgow at COP26.
Heat
Heat-related mortality is becoming evident on every continent, with a recent study attributing 37% of “warm-season heat-related deaths” to anthropogenic climate change. Increases in heat and heatwaves are associated with morbidity and mortality from heat stress and heatstroke, and cardiovascular and respiratory diseases, with the elderly, people with disabilities and outdoor workers most at risk.
Chapter twelve of AR6 assesses specifically the relevance of Climate Impact Drivers (CIDs) for “major categories of sectoral assets” one of which is Health, Wellbeing and Communities. Chapter seven of the IPCC’s Working Group II will provide a full impact assessment, but AR6 provides an indication of the level of confidence from the scientific literature of the impact of CIDs on, and risk to, health. For example, there is high confidence amongst the climate science community that extreme temperatures will exceed “critical thresholds” more frequently by mid-century at 2C of warming, and high confidence that health systems in regions such as South Africa, the Mediterranean, North Central America, Western North America, the Amazon regions, South-western South America, and Australia will be challenged by drought aridity and forest fire (ibid). Moreover, there is high confidence that no region of the world will escape “concurrent changes in multiple CIDs by mid-century”.
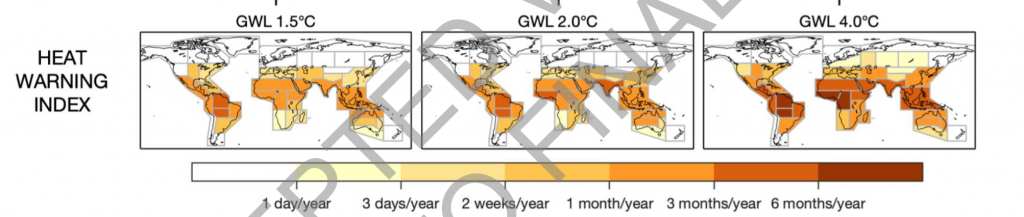
AR6 also utilises a Heat Index used by the United States National Oceanic and Atmospheric Administration (NOAA) to quantify the number of days each year regions could expect a ‘danger level’ heat warning for human health at different levels of global warming – 1.5°C, 2.0°C and 4°C (Fig 1). The rate at which dangerous humid heat thresholds are breached depends on the shared socio-economic pathway (SSP) scenario realised by mid-century but, as an indication, SSP1-2.6 would yield fewer than 50 additional days per year when the temperature exceeds 41°C in some tropical regions while SSP5-8.5 would yield greater than 100 additional days.
Fig 1: Heat Warning Index, AR6
Air pollution
Air pollution killed more than 8.7 million people in 2018, with a higher percentage (31%) of people in Eastern Asia dying than in Europe (17%) or Africa (4%). If air pollution was reduced to levels considered safe by the World Health Organisation people would enjoy on average an additional 2.2 years of life. In some countries, such as India and parts of Nigeria, people would live almost six years longer. Annually, air pollution results in seventeen billion years of life lost.
The relationship between climate change and air pollution is complex. Chapter six of AR6 provides the following summary:
“Climate change and air quality are intimately linked. Many of the human activities that produce long-lived greenhouse gases also emit air pollutants, and many of these air pollutants are also ‘short-lived climate forcers’ that affect the climate. Therefore, many options for improving air quality may also serve to limit climate change and vice versa. However, some options for improving air quality cause additional climate warming, and some actions that address climate change can worsen air quality”.
Reductions in greenhouse gasses (GHG) lead to improved air conditions, which in turn reduces the incidence of a whole range of health conditions. Chapter six notes the synergistic effect of decarbonisation and reduced air pollution. For example, reductions in black carbon and methane would have “substantial co-benefits” because improved air quality would limit the ill-effects on health and make international development targets more feasible (Ch 6.1.2; Cross-chapter Box 1.1).
Chapter six acknowledges the uneven distribution of short-lived climate forcers (SLCFs) across global regions, describing the shift in emissions since the 1990s from North America and Europe to Asia. As noted above, the benefits of cleaner air from reduced emissions would not be enjoyed equally across all global regions. And it warns that in some regions, in the short term, the air quality that would result from even the lowest emissions scenarios (SSP1-2.6 and SSP1-1.9) would not meet World Health Organisation standards (D2.2; Ch6 p6-7).
Chapter six reviews the extent that temperature and air pollution changes can be attributed to different transport sectors, such as aviation, shipping, and land transportation. For example, reducing the sulphur content of marine fuel from 3.5% to 0.5% would reduce sulphate (and consequently PM2.5) and thus reduce the health exposure to PM2.5, especially over India, East China and coastal areas of Africa and the Middle East.
As noted above, the outcome of certain interventions for improving air quality (reduction of particulates in the atmosphere, for example) would, in the short term, cause additional climate warming. In the case of aerosols, for example, chapter six considers both the benefits of reduced aerosols and ozone for health against the ‘disbenefits’ of such reductions for climate change (i.e. increased global warming as less heat is reflected away from Earth). It reports that, under ‘ambitious but plausible’ scenarios, the increase would be a minimal 0.1C.
The section describes both win-win (zero emission vehicles) and win-lose activities (burning wood), policies and behaviours. The FAQ for Chapter six concludes: “Air quality and climate change represent two sides of the same coin, and addressing both issues together could lead to significant synergies and economic benefits while avoiding policy actions that mitigate one of the two issues but worsen the other”.

Forest fires, drought and mental health
In addition to heat and air pollution, physical and mental health are mentioned in the context of forest fires and drought, albeit only briefly. For example, the 2015 drought and forest fires in Indonesia is provided as an example of how the ‘haze crisis’ that resulted impacted negatively on human health. Evidence from the scientific literature provides ‘high confidence’ that “increases in some of the drought, aridity, and fire weather CIDs will challenge, for example, agriculture, forestry, water systems, health and ecosystems…”
Chapter twelve of AR6 refers specifically to mental health in the context of severe storms and the effects of drought on poverty, noting that global warming will increase the incidence of mental health in all regions. The public health community is becoming increasingly aware of the mental health impacts of climate change, as evidenced by the latest Lancet Countdown Commission on Health and Climate Change, which has a new indicator of mental well-being in its 2021 report. No doubt WGII will have much more to say on this issue next year.
Engaging the health community by developing ‘storylines’
The question of how the science community can provide useful climate information for various stakeholders is raised in AR6, and (again) I am certain WGII will have much more to add to this important issue. It concludes that the science community must engage with the health community, its knowledge, and experiences to formulate appropriate information and develop a mutual understanding of the usefulness of the information provided.
Concurrent impacts on health
Although the AR6 WGI report is not required to assess the impacts on or vulnerability to human health from climate change, it nevertheless provides an early indication of how the scientific community and the scientific literature report health and global warming. The take home message for me from this report is that it is crucial to understand the “concurrent impact” that climate impact drivers will have on health in all regions of the world. As the Executive Summary warns: “Every region of the world will experience concurrent changes in multiple CIDs by mid-century (high confidence), challenging the resilience and adaptation capacity of the region”.
It is not simply the case that health systems will have to respond to the effects on population health of just heat or just drought, or provide care to those suffering the effects of mental health. The tragedy of global warming is that these effects will be felt concurrently, adding multiple demands from CIDS simultaneously. Health systems must now prepare to respond to those concurrent challenges.
Andrew
Thanks Andrew,
Very helpful
I await publication of Working Group 2 (early 2022), but predict the health chapter will focus on what Haines et al called the “primary” and “secondary” health effects of climate change, eg heat, infectious diseases and the impacts via air pollution. (That original conceptualisation did not include mental health effects, but I regard them as “cross cutting”).
The “tertiary” consequences are likely to be neglected in the health chapter, as they have in every IPCC health chapter to date. Such effects include from conflict (eg Syrian war, in part), famine and forced displacement. Ultimately, perhaps, the collapse of civilisation.