It’s January, so that can only mean one thing – the first of two annual meetings of the World Health Organisation’s Executive Board. The January meeting is the more important of the two meetings as it’s when the agenda and resolutions of the May World Health Assembly are agreed and adopted. It’s also fun to watch as the members of the Board typically dress up as their favourite Lord of the Rings character and engage in some pretty convincing Tolkein-esque cosplay. Historically, the US member likes to think of themself as The Ring of Power, but this year Admiral Brett Giroir has agreed to dress as Gollum in recognition of his country’s sterling contribution to international cooperation over the past year.
In this post, I reflect on one of two documents presented to the board on WHO financing – EB148/27 Update on the financing and implementation of the Programme budget 2020–2021. In a follow up post, I’ll take a look at EB148/25 Proposed programme budget 2022–2023: Building forward better. Think of these two posts as some ‘looking back’/’looking forward’ reflections on WHO funding pre and (hopefully) post-Covid.
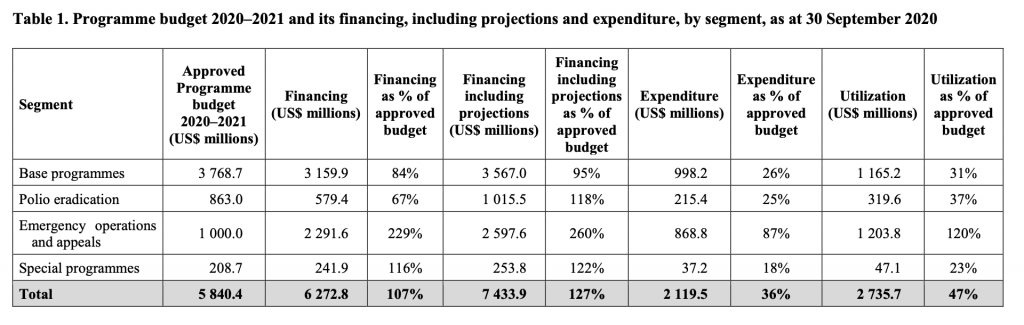
EB148/27 provides a report from the Director General updating the Board on the financing and implementation of the Programme Budget 2020-21, which was approved in May 2019 at WHA72. The total budget for the biennium is US$ 5840.4m, and comprises of 4 ‘segments’: Base programmes = US$3768.7m; Polio eradication = US$863m; Emergency operations and appeals = US$ 1000m; and Special programmes = US$208.7m. EB148/27 is, essentially, Tedros describing to the EB (and therefore accounting for) progress made in financing and implementing the budget during the first 3 quarters of its first year (i.e up to 30th Sept 2020). Table 1 (below) provides a summary of financing and projections for each of the four segments.
Covid impact
This was always going to be a Covid update and the budget reveals the possible impact that Covid is having on WHO budgeting. I think there are at least six indications of Covid impact on WHO financing currently facing the Organisation. I may well be reading too much into these figures, but they certainly warrant further consideration.
We get an indication of what Tedros considers a priority consideration for the Board: unsurprisingly, emergency operations and appeals (segment 3) is foremost in his mind, and this is what he leads with. The first indication of Covid impact, then, is the amount of money allocated to this segment: US$ 3000m (3x the approved level). It’s not clear from the document where Tedros gets the US$3000m figure. Table 1 above has the amount as US$2291.6m financed and US$2597.6m projected. Nevertheless, assuming that US$3 billion is the correct amount, that’s equal to half the entire 2022-23 budget.
The second indication of Covid impact is that projected funds have increased for some segments of the budget but not for others. They have increased by 260% (including projections) for the emergency operations and appeals segment but reduced for the base programmes segment (the 95% figure is lower for 2020-21 compared to the same time in the 2018-19 budget financing cycle, when it was 101% – see EB144/43). Excluding projections, available funding for the base programmes segment is also slightly lower this time around (84%) compared to 2018-19 (89%). Tedros tries to reassure the Board by pointing out that, in absolute terms, more money is available for 2020-21 than was available for 2018-19, but you have to wonder why projections are lower. It’s likely to be that because all eyes are on Covid, other, non-Covid, programmes are simply not receiving as much funding. It’s not a huge difference – 6% and 5% – but still…
The third indication of Covid impact is clearly evident in the polio eradication segment. This has received the least funding so far (67%) because polio staff and assets have been deployed elsewhere to assist in the Covid response. Tedros tries to reassure us with confident words about expecting polio to be more than fully funded by the end of the biennium, but for now it’s definitely not on track.
From the four ‘segments’ of funding, WHO is able to finance its four ‘strategic priorities’ detailed in the Organisation’s 13th General Program of Work (GPW): One billion more people benefiting from universal health coverage; One billion more people better protected from health emergencies; One billion more people enjoying better health and well-being; and a more effective and efficient WHO providing better support to countries. The update informs us that there is a “significant difference” in funding across these strategic priorities (UHC fully funded; health emergencies less than half funded 46%; health and well-being, and WHO reform each just over half funded).
A fourth indication may account for the fact that the health emergencies strategic priority area (one billion more people better protected from health emergencies) is currently under-funded. Tedros is quite nonchalant about this noting what we are seeing “follows the trend of previous bienniums”. Overall, the base budget is not receiving the funding it would normally expect by this point in the funding cycle, which is hampering implementation of programmes. And the explanation for this is Covid: “the implementation of the base budget is delayed due to the large-scale emergency operations in response to the COVID-19 pandemic, as reflected in the emergency operations and appeals segment”. Despite Tedros’ calming words, it’s hard not to conclude that one emergency priority – Covid – is having an impact on the emergency resources available for all the other emergency priorities that WHO has to deal with.
A fifth indication of Covid impact is that travel costs are down by 50% on the 2018-19 biennium, with a saving of US$ 65m. That gives us a rough estimate of business-as-usual travel costs for the Organisation of US$260m (but note the update is good to September 2020 – i.e. not even midway through the biennium – so the figure could be closer to US$300m). WHO is perennially criticised for its travel costs, so Covid may spur further critical reflection on this controversial expense.
Perhaps the most significant – and sixth – indication of Covid impact comes from demand from WHO regional offices. The update has this to say: “As a result of the COVID-19 pandemic response, all major offices show unprecedented levels of emergency operations, appeals financing and utilization, significantly exceeding the amounts estimated under the approved budget”. The demand from LOs far exceeds budget – by 896% for The Americas; 689% for Western Pacific; 310% for Geneva HQ; etc. One has to ask where this money is going to come from?
Covid is clearly having a significant impact on WHO financing, staff and other assets, drawing all away from base programmes, including strategic priority areas. At a time when the world is in the grips of a pandemic, the number of non-Covid emergencies WHO is having to deal with is 3x what it was in 2018-19. As the update notes:“Such an increase in operations inevitably draws on the human resources of the base programmes in addition to the emergency operations and appeals segment of the budget”. Covid is pulling WHO in different directions and it will be very interesting to see the reaction of the Board members to this update.
Somehow, the update ends on a positive note. We are reassured that implementation remains strong, even if it is slowing down. And Tedros lists some mitigation strategies WHO intends to introduce that will ensure 80-85% of projected plans are implemented by the end of 2021. Of course, given the multiple demands on funds, there is one blindingly obvious conclusion which the update doesn’t fail to convey: “the level [of funding] is still not sufficient to ensure equitable financing of all outcomes, major offices and strategic priorities”. Surely, member states will commit to more financial support for the WHO in its hour of need?
Andrew
Great blog Andrew. Its helped me with week 2’s material of the module (Masters Global Health distance learning)
Thanks Christine, glad you found it useful!